We have created some learning resources, including a series of videos featuring exercises and interactive demonstrations, that you can use with your child to help them learn about breathing patterns and breath training, techniques to help control asthma symptoms, and how exercise and physical activity can boost lung health and overall wellbeing.
Click on each heading below to see supportive information, handouts and videos.
Read more about our physiotherapy service for children with asthma.
You will find a video below that is aimed at parents and carers of children with asthma. It will help explain:
- How to spot the signs and symptoms of asthma
- How to identify when difficulty or changes in breathing is asthma or something else
- Common mistakes children can make when trying to identify their symptoms
We have produced a flow chart that you can use to guide you on what to do if your child experiences the onset of asthma or asthma-like symptoms. You can also give this to your child’s teacher or school nurse to help them understand how to help your child when they are feeling breathless.
Please find a useful handout below to help you support your child manage asthma and asthma-like symptoms:
You will find a video series below, containing three short episodes, which will help explain:
- The basics of how we breathe, how our lungs work and how our bodies adapt to exercise
- How some ways of breathing can make symptoms of asthma worse and how to control breathlessness
- How to breathe properly, with an interactive demonstration from Austin (aged 7) and Jessica (aged 9)
Below are some ways to help your child identify their breathing pattern. You can help them do this simple exercise to pay attention to and observe how they breathe. Then, use the list below to spot any similarities with what they noticed about their breathing and compare it to what a good breathing pattern looks like.
Your child may have one, two or all of the things in the table to work on. However, they should just work on one thing at a time.
| Changed breathing pattern | Good breathing pattern |
| Breathing through your mouth (or combination of nose and mouth) | Nose breather |
| Regular sighing, yawning or deeper breaths | Regular gentle rhythm to breathing |
| Breathing to the top of your chest | Breathing to the bottom of your chest |
| You can hear the breath in or out – faster noisy breathing | Slow silent breathing |
| Breath IN is longer than breath OUT | Breath OUT is longer than breath IN |
| Judders in breathing or breath holding | Flowing breath where one breath is similar to the next |
| Tummy muscles tight | Tummy muscles relaxed |
Breathing checklist
- Set a timer for two minutes
- Sit your child down in front of a mirror and have them place one hand across their stomach (like they are giving themselves a hug) and the other on top of their chest
- Start the timer and ask them to carefully observe and feel their breathing
- Ask them the following questions:
- Are you breathing through your nose or your mouth?
- Can you hear your breathing? Is it loud, quiet or silent?
- Are you breathing to the top of your chest or down to your tummy and lower ribs?
- Is there a gentle rhythm to your breathing? Would you compare it to a calm sea or a stormy sea?
- How are you sitting or standing? Are your shoulders round? Is your chin forward? Can you sit up straight with your chin in and shoulders back?
The following video will explain:
- How to go through a breathing pattern checklist
- How to observe your breathing and assess how well your child is breathing
- What signs to look for to work out what is causing your child’s symptoms
Please use the handout below to help guide you through your breathing pattern checklist:
As we explained earlier, symptoms such as shortness of breath, feeling unable to control the breath, and tightness or pain in the chest may present like classic symptoms of asthma but can actually be symptoms of something else, for example stress and anxiety, or dysfunctional breathing. This can make it difficult to pinpoint exactly what is causing the symptoms. However, your child can look for clues to try and work out what is causing certain symptoms, as the video below explains.
The following video will explain:
- How to tell the difference between symptoms of asthma and those which mimic it
- What your child can do to help relieve and manage their symptoms
Please find below some useful handouts to support you with telling symptoms apart:
Feeling breathless can happen for many reasons. For example, your child may feel breathless after exercise, or something stressful or upsetting that makes them breathe faster than normal. But being ‘out of breath’ is different than being ‘short of breath’.
For children with asthma, breathing may feel more difficult in these situations and they may find relief using an asthma inhaler as part of their asthma action plan as instructed by the team involved in their care. If your child does not have an asthma action plan, or you are not sure what this is, please speak with your child’s healthcare team at their next clinic appointment.
If your child feels short of breath after physical activity, there are some simple ‘rescue breathing’ techniques they can do while they wait for their breath to settle. The video below will go through some of these techniques.
The following video will explain:
- Some simple breathing techniques your child can do to help control their breathing when they feel breathless.
Your child can also use the image below as a tool to help control their breathing when they feel breathless. Read the instructions in the green box with them before they start.
![]()
While doing the exercise, assess with your child how they feel every 2-5 minutes – does their breath feel the same, better, or worse? Follow their asthma action plan and seek help when needed.
Once your child’s symptoms have settled, there are things they can do to manage breathlessness and difficulty breathing. You can also speak to your child’s healthcare team for more advice.
Please find below some useful handouts to help with breathlessness:
Posture is the position in which you hold your body. How you breathe can change your posture and your posture can change how you breathe. There is no way to get your breathing perfect if your posture is not right. The trick is to think about this little and often – initially it may not be comfortable to hold a good posture for long if the muscles are not used to holding your body in a certain way. But, if you keep correcting yourself throughout the day, your muscles will adjust and slowly get used to a different posture.
Posture is a bit like the ‘Goldilocks principle’ as told in the story, Goldilocks and the Three Bears - it can take three different forms, with one being ‘just right’.
Too slumped
Shoulders and back rounded and chin poking out. It is hard to breathe down to your lower ribs as they are squashed. In this posture you will tend to breathe to the top of your chest.
Too straight
The back is over-arched, shoulders are up and the tummy is in. Sometimes you might do this when doing lung function or peak flows – but it doesn’t help get bigger numbers.

Just right
Back is straight but keeps its normal curve, shoulders are back and down and the chin is in. The lower ribs are free to move and breathe without being squashed.

Children with asthma may find that their breathing feels fine when they are resting but becomes harder to control when they take part in physical activity.
This could be due to how they are breathing (their breathing pattern) or their fitness level. Understandably, feeling breathless after exercise or physical activity can be uncomfortable, scary and frustrating and, because of this, it is not uncommon for children to reduce their activity, which can lead to a decrease in fitness levels and overall wellbeing.
Research shows that regular exercise improves asthma control. However, we also know that up to a third of people with asthma experience exercise-induced asthma symptoms. But there are steps that can be taken to help reduce the onset of symptoms, including:
- Having an asthma action plan that includes guidance on inhaler use before and/or during exercise
- Learning techniques to control breathing during exercise (see video below)
- Getting advice from your healthcare team (please see contact details below)
The following video will explain:
- How to control breathing during exercise
- How to warm up before exercising, which is essential for keeping control of the breath
- Some moderate to high intensity exercises your child can do, demonstrated by Austin (aged 7), Jess (aged 9) and Charlotte (aged 18)
- How to spot the onset of asthma symptoms, if your breathing pattern is getting worse, or your voice box is tightening, and what to do in each situation.
Please find below some useful handouts to support breathing during exercise:
How to exercise safely
- Please remember that your child’s health and any activity you choose for them to participate in is your responsibility
- If your child is younger than 14 years old, please ensure they do not exercise alone and you or their coach/ instructor is present
- Always ensure that your child is following their personalised asthma action plan and that they have taken their prescribed asthma inhaler(s) (e.g. preventer or reliever inhalers) prior to exercising.
Other things to consider
- Before your child starts any exercise make sure they are feeling well
- Ensure your child is wearing comfortable clothing and supportive footwear
- Make sure there is enough room to exercise safely if exercising indoors/ at home
- Ensure your child is well hydrated, encourage them to have a glass of water before exercising and to keep a bottle of water near them during exercise
- Encourage your child to start exercising gradually, warm up and build up their energy levels during the exercise as they feel comfortable
- If your child is diabetic you should check their blood sugar levels prior to and following exercise and ensure that you have a fast-acting energy snack or drink (e.g. Lucozade), and a slow-acting snack (e.g. a sandwich) to hand if needed.
- Make sure you have your child’s reliever inhaler and spacer to hand, in case they need to use it before, during or after exercise.
- Update the children’s asthma team at Royal Brompton Hospital as well as your child’s GP if there are any changes to your child’s health, for example if they are feeling unwell or any of their medications have changed.
Children with asthma should not start an exercise class if:
- They are feeling unwell with a cough, wheeze, chest pain or temperature
- They have been awake overnight because of their asthma symptoms
- They have been prescribed a new course of steroids (prednisolone) or antibiotics for their asthma
- Their peak flow volumes dropping (if you keep a peak flow diary)
- They have not taken their regular inhaler medications as prescribed, or they have run out of any of their regular or rescue medications
- Their personalised asthma action plan is over a year old.
Identifying a possible asthma attack
Your child should stop exercising and seek help if:
- They cannot talk in full sentences or walk easily because of their breathing
- Their symptoms (wheeze, chest pain, cough) are getting worse quickly
- Their extra reliever inhaler medications are not helping
This advice is in line with the green, amber, red system on your child’s personalised asthma action plan.
Update the children’s asthma team if there has been a change in your child’s treatment, or if they have had a surgical procedure or a hospital admission.
How should activity make your child feel?
Sometimes it is hard to tell the difference between asthma symptoms and what is normal for our breathing when we exercise (link to detailed section on this)
When exercising, your child may feel:
- More breathless, but still able to talk
- Warmer or slightly sweaty
- Their heart beating faster
This is a normal response to physical exertion and does not necessarily indicate symptoms of asthma.
Monitoring the intensity of your child’s activity
When your child is exercising or taking part in physical activity, it is important to measure its intensity to ensure they are safe and get the most benefit out of the activity. For example, if your child is not slightly breathless during exercise, it is likely they are not exercising hard enough. On the other hand, if they cannot talk because they are so breathless, it is likely they are exercising too hard.
The rate of perceived exertion (RPE) scale below can be used to indicate how hard the exercise feels for your child.
You can use the RPE scale with your child and ask how they would score their breathlessness (0-10).
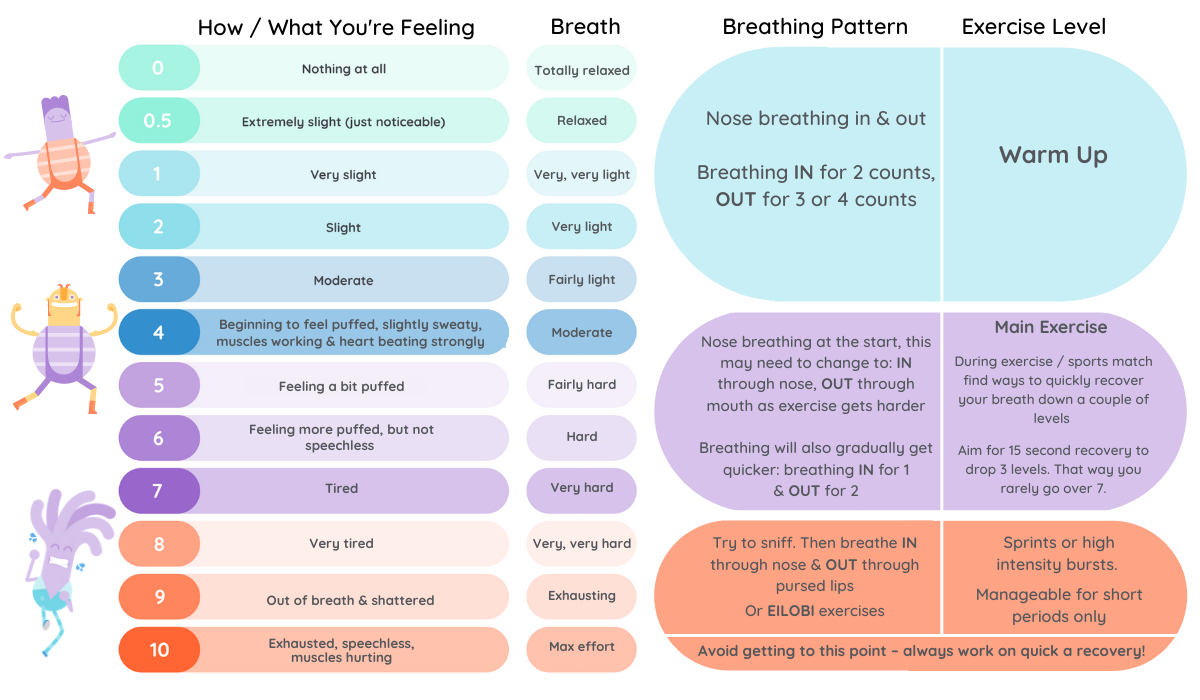
• If the score is less than 4 (i.e. the exercise feels light) you should encourage your child to INCREASE the pace of their exercise.
• If the score is 7 or greater (i.e. the exercise feels hard) you should encourage your child to SLOW the pace of their exercise.
• The score should fall somewhere between 4 and 7.
During exercise sessions...
Your child should slow down if:
- Their breathlessness score is higher than 7 (‘somewhat hard’)
- Their breathing seems very heavy
- They are looking or feeling very tired
Stop if:
- They feel dizzy or nauseous
- They feel clammy or cold
- They get chest pain or tightness, or a new cough
- They feel increasingly wheezy
- A specific exercise increases their pain or discomfort
These signs are an abnormal response to exercise and may indicate that the intensity of the exercise is too high for your child.
Remember, it is normal for your child to feel slightly out of breath when they exercise. They may also feel a little warmer and sweaty. If your child experiences any of the symptoms above, you must discuss this with their asthma team at Royal Brompton Hospital.
If your child experiences chest pain or tightness, or is feeling unwell, they should:
- Stop exercising
- Sit down and rest
- Follow their personalised asthma action plan and take their rescue inhalers using their spacer as prescribed by their healthcare team.
If your child’s symptoms do not subside after following the advice above or they are worsening, seek emergency help.
Below you will find a list of all the handouts associated with this page and sections above. Please click each title to open and download the relevant handout. You can save to your device and also print for your personal use.
- How to help a child when they have asthma or asthma-like symptoms
- Your good breathing checklist
- What could my symptoms be?
- What can I do to help my symptoms go away?
- When you're feeling like a superhero vs when things feel tough
- The 'Take 5' breathing hand for rescue breathing
- Top tips for staying in control of your breathing when exercising
Contact us
The team is led by a lead asthma physiotherapist and supported by the paediatric physiotherapy service at the Royal Brompton Hospital. Please find contact details below.
Phone: 020 7352 8121 extension 82260
Email: gstt.childrensphysio@nhs.net

