How to refer a patient for ECMO
Make a referral using the Signpost ECMO National Referral Pathway website. Please read the instructions carefully.
If you have difficulty in making the referral on the pathway, you can:
- Find referral help on the Signpost ECMO National Referral Pathway website. Get help by clicking “Request Help” (24/7 service)
- Call RBH ECMO Nurse on +44 (0)7815 494 175
Step 2: RBH ECMO team will receive the notification of referral & review the details
Step 3: RBH ECMO Consultant on call will contact the referring doctor and discuss.
If your patient’s condition is time critical, please call the above number while filling the referral.
Referral criteria
During the coronavirus pandemic, patients who meet the following clinical criteria may be considered suitable for ECMO support.
Inclusion Criteria (revised in response to the COVID-19 pandemic)
- Potentially reversible severe respiratory failure
- Lung Injury Score ≥3 (see below)
- Failed trial of ventilation in prone positioning ≥ 6 hrs (unless contraindicated)
- Failed Airway Pressure Release Ventilation (ARPV) or “High PEEP ventilation strategy” ≥ 6 hrs (unless contraindicated)
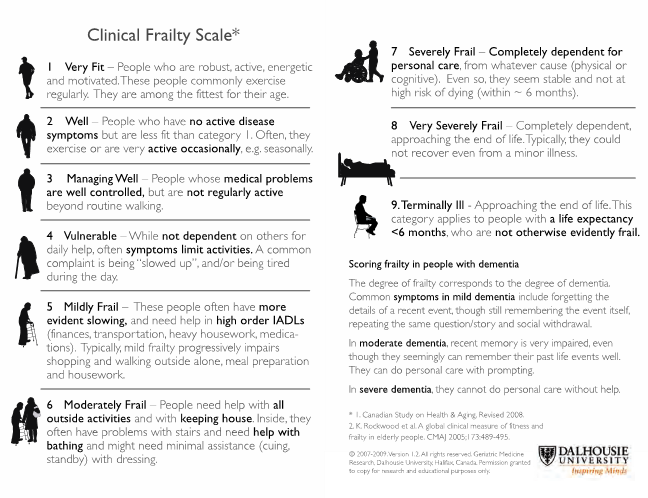
- Clinical Frailty Scale category ≤ 3 (see below)
- If RESP score ≤ 3 ECMO should be considered only after agreement across at least 2 centres
Exclusion Criteria
- Refractory multiorgan failure
Click here for detailed information on the clinical guide for ECMO for respiratory failure in adults during the coronavirus pandemic.
Outside the coronavirus pandemic, the general referring criteria are as follows:
- Severe hypoxaemia (for example, PaO2/FiO2 <13.3kPa)
- Severe hypercapnic acidosis (for example, pH <7.20)
- Inability to achieve lung protective tidal volumes and pressures (tidal volume < 6ml/kg predicted body weight, plateau pressure <30cmH2O)
- Failure to improve with rescue therapies such as high-frequencyoscillation and prone positioning
- Significant air leak/bronchopleural fistula.
There are specific criteria for consideration of ECMO support based on the CESAR study and defined by NHS Specialised Services during the commissioning of ECMO capacity.
Indications | Contraindications (relative) |
|
|
Murray Score (Lung Injury Score)
| 0 | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|
| P/F ratio (kPa)* | ≥40 | 30-39.9 | 23.3 – 29.9 | 13.3 – 23.2 | <13.3 |
| PEEP (cmH2O) | ≤5 | 6-8 | 9-11 | 11-14 | ≥15 |
| Compliance (ml/cmH2O)* | ≥80 | 60-79 | 40-59 | 20-39 | ≤19 |
| CXR quadrants infiltrated | 0 | 1 | 2 | 3 | 4 |
Final Murray Score = Sum of all 4 individual scores divided by 4
* P/F ratio = PaO2/FiO2
* Compliance = Tidal volume (ml) / Driving pressure; Driving pressure = Pplateau – PEEP
Clinical Frailty Scale
Predicted Body Weight & Target Tidal Volume
PBW in kg (males) = 50 + 0.91 x (Height in cm - 152.4)
PBW in kg (females) = 45.5 + 0.91 x (Height in cm - 152.4)
Target TV = 6ml/kg PBW
| Male | Female | |||
| Height | PBW (KG) | Target TV (ml) | PBW (KG) | Target TV (ml) |
| 150 | 47.8 | 287 | 43.3 | 260 |
| 155 | 52.4 | 315 | 47.9 | 288 |
| 160 | 56.9 | 342 | 52.4 | 315 |
| 165 | 61.4 | 369 | 56.9 | 342 |
| 170 | 65.9 | 396 | 61.4 | 369 |
| 175 | 70.5 | 423 | 66.0 | 396 |
| 180 | 75.0 | 450 | 70.5 | 423 |
| 185 | 79.5 | 477 | 75.0 | 450 |
| 190 | 84.2 | 506 | 79.7 | 479 |
