Myocardial disease, bronchiectasis and improving catheter ablations are just some of the themes that have successfully secured funding from a new scheme supported by the Royal Brompton & Harefield Hospitals Charity.
The Research Management Fund, administered by the Research Management Committee (RMC), has been established to help pump prime Royal Brompton and Harefield hospitals based research infrastructure and project grants that strive to tackle heart and lung disease.
The response from RBHH teams to the launch of this scheme was extremely positive and both RMC and the independent panel of expert and lay reviewers were pleased to see this in the breadth and quality of proposals received. 23 applications were submitted for consideration, of which 5 were awarded.
Gill Raikes, who was CEO of the Charity when the scheme was created and has recently retired, said;
“Funding these vital and ground-breaking research programmes is a very exciting project for the Charity, and the Trustees and the team are honoured to be supporting such innovative work.
“Royal Brompton and Harefield hospitals is a centre of excellence for research and knowing that the Charity – our donors and other supporters – can play a part in helping to find treatments and cures for some of these diseases and conditions is inspiring.”
More details on the successful applications are outlined below.
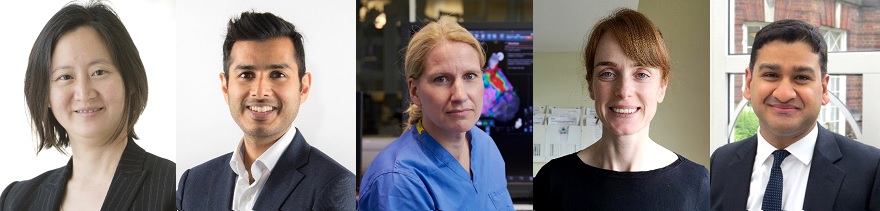
Dr Joyce Wong, consultant cardiologist
Dr Wong’s research team will be using the funds to purchase MRI phantoms which will help to standardise the images taken by MRI scanners, ensuring that any measurements taken are consistent over time and across different machines.
Phantoms are liquid or gel filled objects that are used as stand-ins for human tissue, to ensure that devices and methods for imaging are working correctly. Using phantoms is easier than recruiting large numbers of healthy volunteers or obtaining human tissue.
Dr Wong hopes that this will help with the MRI imaging techniques that measure myocardial scarring (fibrosis) and bruising (oedema) and help cardiologists in the assessment and diagnosis of myocardial disease.
Dr Wong said; “We are really grateful to the Charity for supporting our research. Cardiac MRI T1 and T2 mapping techniques allow us to accurately measure heart damage, and better understand whether the heart is permanently scarred, or only bruised and inflamed. The phantom equipment will help us standardise these measurements across the 5 CMR scanners at our hospitals. This means information from scans of our patients can be compared directly to other international centres, to help design clinical trials of potentially novel treatments.”
Dr Anand Shah, respiratory consultant
Dr Shah’s project aims to determine whether the presence of particular types of bacteria in the airways of patients with bronchiectasis increases the risk of viral infections.
Bronchiectasis is a lung disease where the airways of the lungs become abnormally widened, leading to a build-up of excess mucus that can make the lungs more vulnerable to infection and persistent infections, known as exacerbations.
Individuals with bronchiectasis who have certain bacteria in their airways have an increased number of infections and worse outcome. However, recent research has shown that approximately 50% of these exacerbations may in fact be due to viral infections.
Dr Shah’s team will use nasal samples from individuals with bronchiectasis to determine the effects of different bacteria on the body’s response to viruses and see whether differing responses are the result of effects on immune memory.
The data from the project will be used to help identify new avenues of treatment.
Professor Sabine Ernst, consultant cardiologist
Professor Ernst and her team will be using the funding to carry out a small pilot trial to assess whether catheter ablations can be conducted through the vessels in the arm instead of the groin area.
Catheter ablations usually involve a cardiologist inserting 4 or 5 soft electric wires into the heart via the blood vessels in the groin, with the aim of finding the exact site inside the heart of the patient that is responsible for the ‘electrical fault’.
The team aim to test out a technique using the vessels of the arms rather than the groin, and using 2 electric wires instead of the usual 4 or 5. They have already carried out the procedure successfully on two patients but the funding from the charity will allow for a pilot trial to be conducted that will compare the two methods more robustly.
The team believe the risks for complications will be reduced with the new method, allowing for greater patient comfort during a catheter ablation, and if successful could lead to a reduction in costs thanks to a reduction in the number of catheters needed.
Dr Clare Nolan, specialist pulmonary rehabilitation physiotherapist
Dr Nolan’s study aims to develop a remote pulmonary rehabilitation programme for people with
Interstitial Lung Disease (ILD), a disease characterised by scarring of the lungs that causes breathlessness.
Normally, lung exercise and education programmes (pulmonary rehabilitation) can improve fitness, breathlessness and quality of life in people with different lung disease, including ILD. However, there are problems with programme access and uptake.
So far, research has shown that pulmonary rehabilitation delivered remotely can be beneficial for other lung diseases, but this has not been explored in people with ILD.
The study will interview patients with ILD, carers and pulmonary rehabilitation staff to understand what they believe remote pulmonary rehabilitation for people with ILD should involve. The information will be used to create a specialised programme to be tested as part of a research study.
Dr Shouvik Halder, consultant cardiologist
Dr Haldar and his team will be looking to undertake additional MRI scans of patients with persistent atrial fibrillation undergoing catheter ablations.
The aim will be to determine whether these will help clinicians distinguish better between scar tissue and normal tissue in the heart, allowing for more effective catheter ablation procedures.
Atrial fibrillation (AF) is the most common form of abnormal heart rhythm, with patients usually undergoing a catheter ablation procedure in an attempt to restore a regular heartbeat.
Recently it has been shown that patients with persistent AF have increased scar tissue in their hearts which makes the heart more resistant to treatment. Studies have also shown that in patients for whom this scar tissue is cauterised as part of catheter ablation, the outcomes are improved.
However, it is difficult to differentiate scar tissue from normal tissue which is why Dr Haldar’s study will use MRI scans to assess how the scar pattern evolves after treatment. This will give insights into the effect of treatment and the potential mechanisms of AF reoccurring after ablation.
The study’s ultimate aim will be to improve outcomes and minimise the need for repeat procedures
