 Big data, the role of alcohol in dilated cardiomyopathy and the emerging sub-speciality of cardio-oncology - were all on the agenda at The Institute of Cardiovascular Medicine and Science (ICMS) annual symposium, held at The Royal College Physicians.
Big data, the role of alcohol in dilated cardiomyopathy and the emerging sub-speciality of cardio-oncology - were all on the agenda at The Institute of Cardiovascular Medicine and Science (ICMS) annual symposium, held at The Royal College Physicians.
A partnership between Royal Brompton & Harefield NHS Foundation Trust (RB&HFT) and Liverpool Heart and Chest Hospital NHS Foundation Trust, the ICMS is a world-class body which aims to deliver clinical research programmes that translate directly into clinical practice.
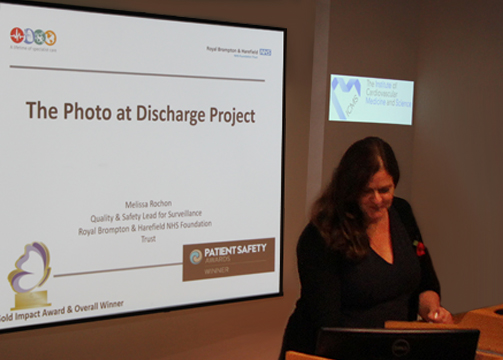
After an introduction from Professor Rod Stables, consultant cardiologist and director of interventional cardiology services at the Liverpool Heart and Chest Hospital, the first speaker, Melissa Rochon, clinical nurse specialist at Harefield Hospital, discussed the 'Photo at Discharge' project, a simple yet effective innovation which allows clinicians to monitor wound healing more effectively.
This was followed by presentations from Harefield’s Dr Miles Dalby consultant cardiologist (RB&HFT), and Dr Rob Cooper, formerly of Liverpool Heart and Chest Hospital, who now consults at Royal Brompton.
Other highlights included Dr Archie Rao’s insight into cardiac pacing and an overview by Dr Ed Conley, from technology company AIMES, on how data is shaping medicine and research.
Dr Alex Lyon, who set up the UK’s first cardio-oncology clinic, a joint venture between Royal Marsden and Royal Brompton hospitals, gave an overview on the birth of this new sub-speciality.
“More and more people are surviving cancer, thanks to new treatments, such as targeted molecular therapies,” he told the audience. “However, the consequence of this is we’re now seeing many more people with heart problems related to cardiotoxicity from cancer treatments; things are getting more complex.”
Dr Lyon underlined the importance of cardiologists working with other disciplines. “When you tell oncologists and haematologists that you can help their patients survive, they start to listen. The good news is, ninety per cent of patients who develop cardiotoxicity during cancer treatment, completed their treatment.”
Dr Shelley Rahman Haley, clinical lead for echocardiography (Harefield Hospital), added: “Advances in treatments mean for some, we are reaching a stage where cancer may be a condition you live with, rather than die from. This is good news – but it brings new challenges and things are moving very fast.”
Professor Sanjay Prasad (RB&HFT) gave an update on the latest research into dilated cardiomyopathy.
He commented: "The latest research – including the discovery of the Titin gene – means we have a much greater understanding of what triggers dilated cardiomyopathy. It can be genetic, or alcohol-related. For example, we have discovered that men seem to be more at risk. Our findings are helping us identify who should and shouldn't have more extensive treatment.”
After a presentation by Dr Tim Fairburn of Liverpool Heart and Chest Hospital on non-invasive fractional flow reserve, delegates were given an overview of future developments and aspirations from Professor Thomas Lüscher, director of education, research and development at RB&HFT, and Professor Gregory Lip, newly appointed honorary consultant cardiologist at Liverpool Heart and Chest Hospital.
Professor Lüscher told the audience that a primary focus for the future is collaborative clinical research, working together with Liverpool Heart and Chest Hospital and other partners. He said: “Registries and biobanks are going to be key to this; they’re not randomised, but they give insights into the natural history and real-world data. You can look at the successes – what works and what doesn’t.”
